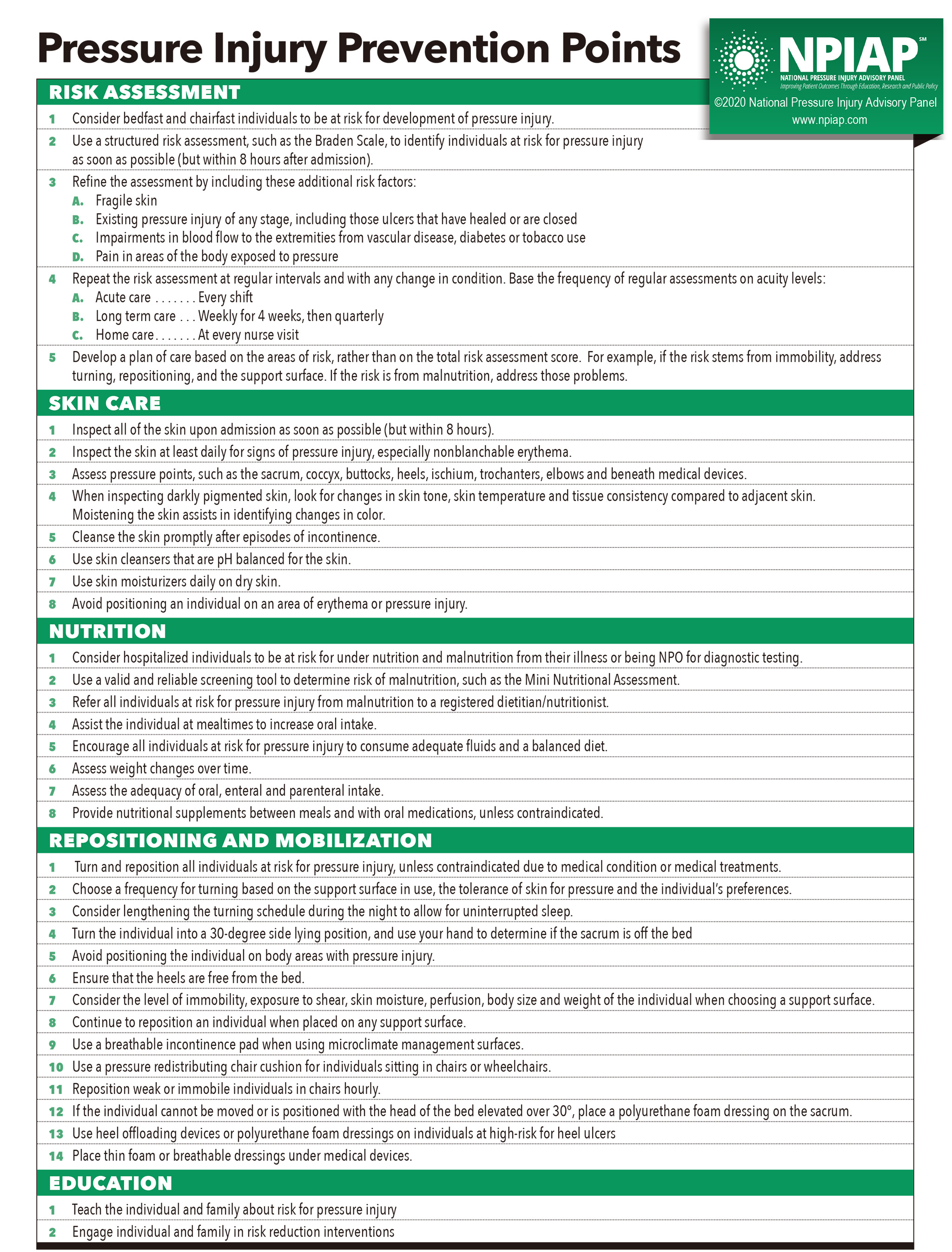
Pressure Injury Prevention Points
Risk Assessment
- Consider bedfast and chairfast individuals to be at risk for development of pressure injury.
- Use a structured risk assessment, such as the Braden Scale, to identify individuals at risk for pressure injury as soon as possible (but within 8 hours after admission).
- Refine the assessment by including these additional risk factors.
- Fragile skin
- Existing pressure injury of any stage, including those ulcers that have healed or are closed
- Impairments in blood flow to the extremities from vascular disease, diabetes or tobacco use
- Pain in areas of the body exposed to pressure
- Repeat the risk assessment at regular intervals and with any change in condition. Base the frequency of regular assessments on acuity levels:
- Acute care… Every shift
- Long term care… Weekly for 4 weeks, then quarterly
- Home care… At every nurse visit
- Develop a plan of care based on the areas of risk, rather than on the total risk assessment score. For example, if the risk stems from immobility, address turning, repositioning, and the support surface. If the risk is from malnutrition, address those problems.
Skin Care
- Inspect all of the skin upon admission as soon as possible (but within 8 hours).
- Inspect the skin at least daily for signs of pressure injury, especially nonblanchable erythema.
- Assess pressure points, such as the sacrum, coccyx, buttocks, heels, ischium, trochanters, elbows and beneath medical devices.
- When inspecting darkly pigmented skin, look for changes in skin tone, skin temperature and tissue consistency compared to adjacent skin. Moistening the skin assists in identifying changes in color.
- Cleanse the skin promptly after episodes of incontinence.
- Use skin cleansers that are pH balanced for the skin.
- Use skin moisturizers daily on dry skin.
- Avoid positioning an individual on an area of erythema or pressure injury.
Nutrition
- Consider hospitalized individuals to be at risk for under nutrition and malnutrition from their illness or being NPO for diagnostic testing.
- Use a valid and reliable screening tool to determine risk of malnutrition, such as the Mini Nutritional Assessment.
- Refer all individuals at risk for pressure injury from malnutrition to a registered dietitian / nutritionist.
- Assist the individual at mealtimes to increase oral intake.
- Encourage all individuals at risk for pressure injury to consume adequate fluids and a balanced diet.
- Assess weight changes over time.
- Assess the adequacy of oral, enteral and parenteral intake.
- Provide nutritional supplements between meals and with oral medications, unless contraindicated.
Repositioning and Mobilization
- Turn and reposition all individuals at risk for pressure injury, unless contraindicated due to medical condition or medical treatments.
- Choose a frequency for turning based on the support surface in use, the tolerance of skin for pressure and the individual’s preferences.
- Consider lengthening the turning schedule during the night to allow for uninterrupted sleep.
- Turn the individual into a 30-degree side lying position and use your hand to determine if the sacrum is off the bed.
- Avoid positioning the individual on body areas with pressure injury.
- Ensure that the heels are free from the bed.
- Consider the level of immobility, exposure to shear, skin moisture, perfusion, body size and weight of the individual when choosing a support surface.
- Continue to reposition an individual when placed on any support surface.
- Use a breathable incontinence pad when using microclimate management surfaces.
- Use a pressure redistributing chair cushion for individuals sitting in chairs or wheelchairs.
- Reposition weak or immobile individuals in chairs hourly.
- If the individual cannot be moved or is positioned with the head of the bed elevated over 30º, place a polyurethane foam dressing on the sacrum.
- Use heel offloading devices or polyurethane foam dressings on individuals at high-risk for heel ulcers.
- Place thin foam or breathable dressings under medical devices.
Education
- Teach the individual and family about risk for pressure injury.
- Engage individual and family in risk reduction interventions.