What is support Surfaces?
Support surfaces are specialized devices for pressure redistribution designed for management of tissue loads, microclimate, and/or other therapeutic functions (i.e., any mattress, integrated bed system, mattress replacement, overlay, or seat cushions, or seat cushion overlay).
What benefits of using support Surfaces?
In this context, pressure refers to distribution of forces on the individual’s body surface that is in contact with the device. As a person immerses (sinks) into the support surface, their weight can become distributed over a larger area. If the surface also envelops (i.e. conforms to the shape of) the person, the pressure on the individual’s body will become more evenly distributed and less concentrated over bony prominences where pressure ulcers typically develop.
In practice, as a person lies or sits on a support surface their weight causes both the support surface and their own soft tissue to deform. The extent to which pressure is concentrated over small areas will determine the degree of potentially damaging deformation.
A reactive support surface is a powered or non-powered support surface with the ability to change its load distribution properties only in response to an applied load.
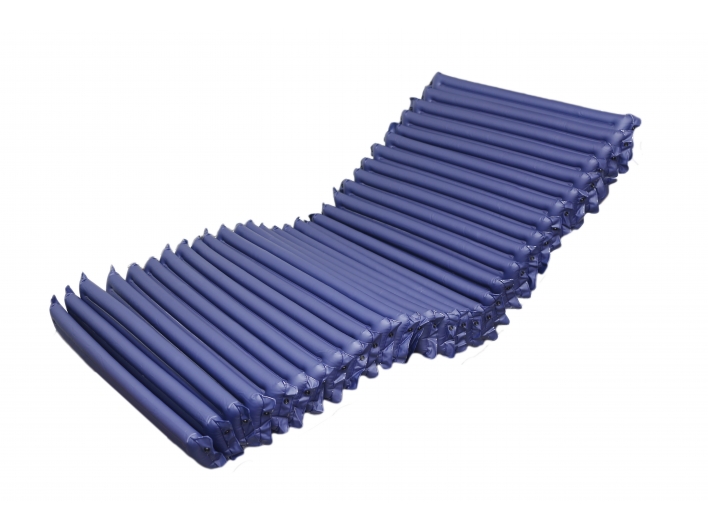
An active support surface is a powered support surface that produces alternating pressure through mechanical means and has the ability to change its load distribution properties with or without an applied load.
What sorts of support surface?
Support surfaces are typically constructed from a range or combination of material including foam, gel and fluid, and structures (i.e., bladders and modules that may be arranged in zones corresponding to anatomical location).
Pressure ulcer risk factors vary from person to person. Support surfaces should be chosen on an individual basis depending on these personal needs. In all cases, the manufacturer’s recommendations for the use and maintenance should be followed. Standards also serve manufacturers as a product development guide and to enhance quality assurance.
Microclimate refers to the temperature and humidity of the interface between the support surface and the individual. Pressure distribution, shear management and microclimate influence a person’s risk of developing a pressure ulcers.
Reactive support surfaces are designed to reduce the risk of pressure ulcer development by deforming in response to applied load(i.e., the individual’s weight and/or morphology). The goal is to provide deep immersion and a high degree of envelopment to reduce sustained deformation caused by pressure concentrations over bony prominence.
Active support surfaces are design to reduce the risk of pressure ulcer development by periodically shifting the areas of support from between anatomical locations so that deformation is not sustained over any one area. The weight-shifting feature is typically achieved by cycling air into and out of bladders within the support surface. This feature is called alternating pressure.
Later rotation, percussion and vibration are examples of therapeutic functions of support surfaces that are not intended to reduce pressure ulcer risk.
Support Surface USE
Support surfaces are an important element in pressure ulcer treatment because they provide an environment that enhances perfusion of injured tissue. Support surfaces alone neither prevent no heal pressure ulcers. They are to be used as part of total management plan for pressure for pressure ulcer prevention and treatment.
General Recommendations for mattress and bed Support Surfaces
1. Select a Support surface that meets the individual ‘s needs. Consider the individual’s need for pressure redistribution based on the following factors:
。 level of immobility and inactivity;
。need for microclimate control and shear reduction;
。size and weight of the individual;
。risk for development of new pressure ulcers; and
。number, severity, and location of existing pressure ulcers.
This statement is based on expert opinion. Immobility is the key condition that increases risk of pressure ulcers. This risk in increased when immobile individuals are too weak to turn or reposition themselves, are experiencing pain and discomfort on movement, or when they are unaware of the need to move about in bed. Individuals who must have the head of the bed elevated for medical purposes may benefit from shear reduction from microclimate control. Individuals with damp skin (e.g., commonly from perspiration, fever and incontinence) may benefit from microclimate control.
Selection of Support surface should consider the individual’s body dimensions, ensuring there is adequate spare for repositioning.
Individual should not lie on a pressure ulcer; however, there are instance where the individual cannot be positioned off the ulcer and instance because the individual has ulcers on multiple anatomical sites. To improve perfusion to injured skin and existing pressure ulcers, support surfaces with additional features(e.g., alternating pressure, low-air-loss or air fluidized) maybe needed for individuals with existing full thickness ulcers(i.e.,Category/Stage III, IV and unstageable pressure ulcers), while other support surfaces may suffice for partial thickness pressure ulcers(i.e., Category/Stage I and II pressure Ulcers).
2. Choose a support surface that is compatible with the care setting.
This statement is based on expert opinion. When selecting a support surface, consideration should be given to where the support surface and/or bed will be placed. Consider the weight of the bed, the structure of the building, the width or doors, the availability of uninterrupted electrical power, and safe location for the pump/motor, including ventilation. Plans should be in place for the contingency of power failure.
Caregivers should follow supplier’s instructions regarding maintenance schedules and care and use of the support surface. To prevent falls, electrical cords should be kept away from transfer/walk areas. Support Surface pumps/motor should not be obstructed by pillows, bedding, blankets, or clothing. The obstructed motor may overheat and fail to operate.
3. Examine the appropriateness and functionality of the support surface on every encounter with the individual.
This statement is based on expert opinion. It is difficult to determine whether the chosen support surface will work for given person until that individual is actually on the support surface. Any support surface can fail or be less than adequate for an individual’s needs. Caregivers must monitor for power failure and bottoming out and implement the contingency plan if needed.
4. Identify and prevent potential complications of support surface use.
Proper selection and operation of support surfaces is the key to preventing complications. Correctly fitting the mattress to the bed base will mitigate entrapment risks. Overlays placed on top of existing mattresses can elevate the surface to the level of side rails. The top of the side rail should be more than 220mm(8.66iches)above the uncompressed mattress(international Electro technical commission[IEC]60601-2-52). The additional height may make it difficult to transfer onto the bed from a seated position. High beds may be difficult to get out of, increasing the risk of falling and injury.
Beds that produce air flow at the skin interface can accelerate the evaporation of perspiration and can in some case lead to dehydration. This insensible loss should be considered in daily fluid intake. Beds that lead to a sensation of floating may lead to disorientation and confusion; in such cases, reorientation and explanations of the bed’s function may be helpful. Powered support surfaces can be noisy, may generate heat, and can have motion.
5. Verify that the support surface is being used within its functional life span, as indicated by the manufacturer’s recommended test method.
It is widely recognized that support surfaces have a finite life span. Determining the condition of a support surface can be accomplished through contractual support surface performance verification conducted by the manufacturer, or by hospital staff trained in the use of industry recognized test methods.
6. Continue to reposition individuals placed on a pressure redistribution support surface.
This statement is based on expert opinion. Repositioning is still required for pressure relief and comfort when a support surface is in use. However, the frequency of repositioning may alter as a result of using a support surface.
7. Choose positioning devices and incontinence pads, clothing and bed linen that are compatible with the support surface. Limit the amount of linen and pads placed on the beds.
This statement is based on expert opinion. Devices with sharp edges should not be used near Support Surfaces.
Believe that you could select a fit and comfort support surface when you grasp these recommendation point.
Referred:
National Pressure Ulcer Advisory Panel (NPUAP)’s Clinical Practice Guideline.